GHANA: A PROPOSAL TO PRAY AND PAY FOR
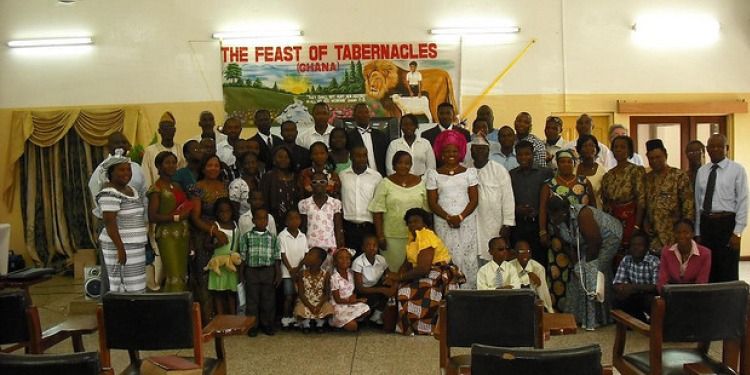 By Melanie ThompsonContributing WriterThe country of Ghana, inhabited by 21.6 million individuals, has been hailed as a democratic success, economically prevailing in the exploitation of its resources. Given its vast wealth as a result of extractable raw materials such as cocoa, gold and timber, Ghana is a true success story of its colonial legacy of exportation (Central Intelligence Agency). Despite its economic success, Ghana has an inhumane form of treatment for its citizens with mental disabilities.Of the 21.6 million citizens of Ghana, it is estimated that 2.8 million of them suffer from mental disabilities (“Ghana Grapples with Mental Health | Human Rights Watch.”). Of this 2.8 million, only two percent are receiving any kind of formal treatment, meaning care within a state monitored facility or a state licensed psychiatric care professional ("Mental Health Society of Ghana.”). The other 98 percent without access to proper treatment options are typically citizens who live in in the inland or northern regions of Ghana, as the majority of care facilities are conglomerated around the urban center of Accra. The options for this large portion of the population are limited: migrate to one of Ghana’s overcrowded state facilities, consult a traditional healer, suffer in silence, or worse, be treated in one of Ghana’s rural prayer camps.Medi Ssengooba described his experience with Ghana’s mental care institutions when reporting and writing for CNN. As a citizen of Uganda, he had been optimistic due to the country’s economic and democratic success. Originally shocked by the substandard conditions in government sanctioned psychiatric care facilities, which included ratios around four staff to every two thousand patients and unsanitary living situations, it was the privately owned Christian, religious institutions that mortified this reporter. At one of the facilities, he interviewed a child named Elijah whose treatment for insomnia was being chained to a tree. Elijah’s parents had forced him into the care institution five months prior , where he been waiting until the “prophet” deemed him cured. Like Elijah, a majority of the individuals housed at the Jesus Divine Temple, also known as the Nyakumasi Prayer Camp, lived without shelter, were malnourished, and are held there involuntarily until they are “cured” (Ssengooba) In another prayer camp, called Mount Horeb, individuals lived in cells without walls, guards, or bars. It was two meter long chains clasped to their person that forced them to bathe, defecate, eat, and sleep all within that 2-meter radius which dictated their “cells”. These patients were left there for weeks or months at a time (Burke).The conditions that are seen in the psychiatric care facilities and, more specifically, in the privately owned prayer camps are in direct violation of article five in the Universal Declaration of Human Rights. Article Five states, “No one shall be subjected to torture or to cruel, inhuman, or degrading treatment or punishment.” The conditions, under which the patients are held, within areas that contain their own urine and feces and without food or shelter, are inhumane and degrading treatments. Moreover, they are involuntarily being subject to treatments that are clearly a form of torture.With the economic and democratic successes that are seen in Ghana, it is hard for the committee to understand how the treatment of Ghana’s citizens with mental disabilities has reached such extreme conditions. The Ministry of Health must make this issue of psychological health a highlighted discussion topic on their annual agenda. They must follow through with the initiative of passing the Mental Health Bill and support the bill with the necessary funding to provide sufficient services to its citizen outside of the central populated area of Accra. Moreover, the Ministry of Health must demand that the government to monitor the prayer camps and shut down facilities that are in violation of the human rights laws agreed upon within the Universal Declaration of Human Rights. Lastly, the Ministry of Health needs to promote mental disorders as medical illnesses, not spiritual corruption—to encourage citizens to seek professional help over traditional practices. Without these policy changes, the citizens of Ghana will be left without any medical alternatives to these prayer camps which subject them to extreme violations of their human rights when suffering from mental illness. If there is no change, these camps will continue to operate, expand and inflict permanent damage upon those individuals with mental health disorders and the stigma that surrounds them.It is easy to tell them to simply shut down the prayer camps. To stop operation would require the manpower to shut the camps down. Moreover, it would require monitoring to keep them from reopening. Once shut down, Ghana must deal with the displacement of the individuals who were held at those camps. However, this is not to say nothing should be done. On the contrary, this is to support the argument that the effort put into the policy must be strong enough to handle the backlash as well as complex enough to solve the initial problems that caused the prayer camps: the insufficient mental care facilities and resources.A policy proposal that has been discussed in regards to Ghana involves a combination of traditional and conventional health care methods. In this policy proposal, Kenneth Ae-Ngibise affirms the suggestion that traditional practitioners, commonly referred to as healers, prophets or the more western, colloquial term “witch doctors,” tend to patient care and if traditional measures do not terminate the patients’ problems, the traditional healer will refer him to the conventional practitioner in the area. The authors argue that the combination of these two groups would lead to limiting the human rights abuses occurring in the traditional “healing centers” without forcing citizens to abandon their cultural connection with these traditional medicines (Ae-Ngibse, Kenneth).The positives of this proposal cannot be denied. It would require less of the state, as it would not need to build more psychiatric facilities; it minimizes the cost and travel for individuals to seek help and keeps intact cultural traditions found in these medicinal practices. However, the main flaw to this proposal is that it generates too much resistance between traditional and conventional medical practitioners. “Some steps have been taken to try and form collaborations between more conventional psychiatric services, and traditional and faith healer practices in Ghana, but these have been largely unsuccessful” (Ae-Ngibse, Kenneth, 559). Traditional practitioners are resistant to work with conventional doctors as they come from different ideologies; moreover, they have their own referral systems within the circle of traditional healers. On the other hand, conventional practitioners do not want to collaborate because they see it as a breach of ethics to oversee the healing of patients through traditional means that they may deem harmful, unhelpful and, in some extremes, a violation of human rights.Ghana has taken a large leap forward in terms of policy regarding the mental health institutions. On August 2, 2012 the Mental Health Bill,a bill that has been in the works since its introduction into parliament during 2004,finally passed. This bill is reported to protect individual’s rights in both state and privately owned facility, but the official documentation has not been made currently available (Parliament Passes Mental Health Bill). Undeniably, this is a step in the correct direction for Ghana’s government. However, it took the Mental Health Bill eight years to pass and it is expected to take even longer than that to be put into effect. Its weakness is in its lack of support, the minimal amount of urgency the issue is seen as, and the insufficiency in the bills funding.It has been clearly demonstrated that the cases of the human rights violations that are occurring within these prayer camps are a direct violation to the Universal Declaration of Human Rights. The committee has explained that the cause of these atrocities are easily pinned to the insufficient mental care facilities and resources being provided. The Committee of the Rights of Persons with Disabilities should propose a conjunctive policy that seeks to remedy the lack of funding as a conjunctive aid to the Mental Health Bill.“There are 600 psychiatric nurses instead of the over 3,000 needed; 115 community psychiatric nurses instead of over 3,000 required, and with only three psychiatric hospitals operating in the country” (Amoah). For these gaps to be met, the Ministry of Health must increase its budget allotted to the maintenance and more importantly the improvement of the facilities the state owns. During the fiscal year of 2007-2008 the Ministry of Health only allotted 3.95% of its budget towards mental health. That means $17,412,263 was spent that year.In a quick glance, that figure may seem like a large sum, however when broken down it means the government only spent 76 cents per capita (Raja, Shoba). The budget, within this policy, would be mandated to renovate three existing psychiatric facilities and to begin the construction of two new mental health treatment centers. It would be realistic to assert that this process would be laid out on a multiple year timeline. The most important intervention must be done within the prayer camps that are committing crimes against human rights. The renovation of the three current facilities should be timed one after the other, so only one will experience closures at any given time. Moreover, it is important that the budget continue to grow to meet the needs as Ghana transitions from three facilities to five.As it would it would be ideal for this policy to mandate to the immediate cease and closure of all prayer camps found to be in violation of human rights, however, those displaced from this closure would be refugees as they were often abandoned there in the first place. It is the recommendation of the Committee that the camps be placed on close monitoring and probation with immediate closure if crimes continue. A policy plan, that has proven successful, is to increase the amount of professionals within the country to monitor and improve these institutions. The policy did this by encouraging graduate psychology students to spend a year abroad within a developing country. By doing so, they can obtain hands on experience, complete research, and invest in the mental health capacity (Patel). This will bring in experienced conventional practitioners into the country on the University’s budget and will help reach the satisfactory amount of professionals needed to allow the individuals left at these camps to receive proper care until Ghana’s facilities can meet their citizens needs.It stands to reason that privately owned institutions and traditional practitioners who are not found to be violation of human rights may remain open but they must remain in accord with the Universal Declaration of Human Rights. Ideally, this monitoring and guidance could come from the individuals study abroad program as proposed earlier. Without the increase in capacity of Ghana’s mental health care facilities prayer camps will still arise to fill the unmet need of the citizens. options. Moreover, this policy will ensure that the funding is being used to spread the facilities throughout the inland and northern regions where prayer camps are the most common.BibliographyAe-Ngibse, Kenneth. "A Qualitative Exploration into the Widespread Use of Traditional andFaith Healers in the Provision of Mental Health Care in Ghana. “International Review of Psychiatry 22.6 (2010): 558-67. Print.Amoah, Anthony. "Four Psychiatrists for over 2 Million Mental Patients?" Ghanaian Chronicle.Web. 14 Nov. 2012.Burke, Laura. "Ghana Mental Hospital Patients Abused, Says Human Rights Watch."Huff PostWorld."Central Intelligence Agency." CIA. WORLD FACTBOOK, Web. 13 Nov. 2012.Laugharne, Richard, and Tom Burns. "The Psychiatrist." Mental Health Services in Kumasi,Ghana. 1999. 13 Nov. 2012.Medi Ssengooba "Ghana Grapples with Mental Health | Human Rights Watch." Human RightsWatch. Web. 13 Nov. 2012.“Mental Health Society of Ghana." Welcome to MHSOG. Web. 13 Nov. 2012.Patel, Virkman "Returning the Debt: How Rich Countries Can Invest in Mental Health Capacityin Developing Countries." Perspective: National Center for Biotechnology Information."Parliament Passes Mental Health Bill | Health." Parliament Passes Mental Health Bill | Health.Web. 14 Nov. 2012.Raja, Shoba. "Mapping Mental Health Finances in Ghana, Research Uganda, Sri Lanka, Indiaand Lao PDR." International Journal of Mental Health Systems 4.11 (2010)AppendicesUN General Assembly, Universal Declaration of Human Rights, 10 December 1948, 217 A (III), available at: http://www.unhcr.org/refworld/docid/3ae6b3712c.html [accessed 15 November 2012]Article 5.No one shall be subjected to torture or to cruel, inhuman or degrading treatment or punishment.Photo by tatteralan
By Melanie ThompsonContributing WriterThe country of Ghana, inhabited by 21.6 million individuals, has been hailed as a democratic success, economically prevailing in the exploitation of its resources. Given its vast wealth as a result of extractable raw materials such as cocoa, gold and timber, Ghana is a true success story of its colonial legacy of exportation (Central Intelligence Agency). Despite its economic success, Ghana has an inhumane form of treatment for its citizens with mental disabilities.Of the 21.6 million citizens of Ghana, it is estimated that 2.8 million of them suffer from mental disabilities (“Ghana Grapples with Mental Health | Human Rights Watch.”). Of this 2.8 million, only two percent are receiving any kind of formal treatment, meaning care within a state monitored facility or a state licensed psychiatric care professional ("Mental Health Society of Ghana.”). The other 98 percent without access to proper treatment options are typically citizens who live in in the inland or northern regions of Ghana, as the majority of care facilities are conglomerated around the urban center of Accra. The options for this large portion of the population are limited: migrate to one of Ghana’s overcrowded state facilities, consult a traditional healer, suffer in silence, or worse, be treated in one of Ghana’s rural prayer camps.Medi Ssengooba described his experience with Ghana’s mental care institutions when reporting and writing for CNN. As a citizen of Uganda, he had been optimistic due to the country’s economic and democratic success. Originally shocked by the substandard conditions in government sanctioned psychiatric care facilities, which included ratios around four staff to every two thousand patients and unsanitary living situations, it was the privately owned Christian, religious institutions that mortified this reporter. At one of the facilities, he interviewed a child named Elijah whose treatment for insomnia was being chained to a tree. Elijah’s parents had forced him into the care institution five months prior , where he been waiting until the “prophet” deemed him cured. Like Elijah, a majority of the individuals housed at the Jesus Divine Temple, also known as the Nyakumasi Prayer Camp, lived without shelter, were malnourished, and are held there involuntarily until they are “cured” (Ssengooba) In another prayer camp, called Mount Horeb, individuals lived in cells without walls, guards, or bars. It was two meter long chains clasped to their person that forced them to bathe, defecate, eat, and sleep all within that 2-meter radius which dictated their “cells”. These patients were left there for weeks or months at a time (Burke).The conditions that are seen in the psychiatric care facilities and, more specifically, in the privately owned prayer camps are in direct violation of article five in the Universal Declaration of Human Rights. Article Five states, “No one shall be subjected to torture or to cruel, inhuman, or degrading treatment or punishment.” The conditions, under which the patients are held, within areas that contain their own urine and feces and without food or shelter, are inhumane and degrading treatments. Moreover, they are involuntarily being subject to treatments that are clearly a form of torture.With the economic and democratic successes that are seen in Ghana, it is hard for the committee to understand how the treatment of Ghana’s citizens with mental disabilities has reached such extreme conditions. The Ministry of Health must make this issue of psychological health a highlighted discussion topic on their annual agenda. They must follow through with the initiative of passing the Mental Health Bill and support the bill with the necessary funding to provide sufficient services to its citizen outside of the central populated area of Accra. Moreover, the Ministry of Health must demand that the government to monitor the prayer camps and shut down facilities that are in violation of the human rights laws agreed upon within the Universal Declaration of Human Rights. Lastly, the Ministry of Health needs to promote mental disorders as medical illnesses, not spiritual corruption—to encourage citizens to seek professional help over traditional practices. Without these policy changes, the citizens of Ghana will be left without any medical alternatives to these prayer camps which subject them to extreme violations of their human rights when suffering from mental illness. If there is no change, these camps will continue to operate, expand and inflict permanent damage upon those individuals with mental health disorders and the stigma that surrounds them.It is easy to tell them to simply shut down the prayer camps. To stop operation would require the manpower to shut the camps down. Moreover, it would require monitoring to keep them from reopening. Once shut down, Ghana must deal with the displacement of the individuals who were held at those camps. However, this is not to say nothing should be done. On the contrary, this is to support the argument that the effort put into the policy must be strong enough to handle the backlash as well as complex enough to solve the initial problems that caused the prayer camps: the insufficient mental care facilities and resources.A policy proposal that has been discussed in regards to Ghana involves a combination of traditional and conventional health care methods. In this policy proposal, Kenneth Ae-Ngibise affirms the suggestion that traditional practitioners, commonly referred to as healers, prophets or the more western, colloquial term “witch doctors,” tend to patient care and if traditional measures do not terminate the patients’ problems, the traditional healer will refer him to the conventional practitioner in the area. The authors argue that the combination of these two groups would lead to limiting the human rights abuses occurring in the traditional “healing centers” without forcing citizens to abandon their cultural connection with these traditional medicines (Ae-Ngibse, Kenneth).The positives of this proposal cannot be denied. It would require less of the state, as it would not need to build more psychiatric facilities; it minimizes the cost and travel for individuals to seek help and keeps intact cultural traditions found in these medicinal practices. However, the main flaw to this proposal is that it generates too much resistance between traditional and conventional medical practitioners. “Some steps have been taken to try and form collaborations between more conventional psychiatric services, and traditional and faith healer practices in Ghana, but these have been largely unsuccessful” (Ae-Ngibse, Kenneth, 559). Traditional practitioners are resistant to work with conventional doctors as they come from different ideologies; moreover, they have their own referral systems within the circle of traditional healers. On the other hand, conventional practitioners do not want to collaborate because they see it as a breach of ethics to oversee the healing of patients through traditional means that they may deem harmful, unhelpful and, in some extremes, a violation of human rights.Ghana has taken a large leap forward in terms of policy regarding the mental health institutions. On August 2, 2012 the Mental Health Bill,a bill that has been in the works since its introduction into parliament during 2004,finally passed. This bill is reported to protect individual’s rights in both state and privately owned facility, but the official documentation has not been made currently available (Parliament Passes Mental Health Bill). Undeniably, this is a step in the correct direction for Ghana’s government. However, it took the Mental Health Bill eight years to pass and it is expected to take even longer than that to be put into effect. Its weakness is in its lack of support, the minimal amount of urgency the issue is seen as, and the insufficiency in the bills funding.It has been clearly demonstrated that the cases of the human rights violations that are occurring within these prayer camps are a direct violation to the Universal Declaration of Human Rights. The committee has explained that the cause of these atrocities are easily pinned to the insufficient mental care facilities and resources being provided. The Committee of the Rights of Persons with Disabilities should propose a conjunctive policy that seeks to remedy the lack of funding as a conjunctive aid to the Mental Health Bill.“There are 600 psychiatric nurses instead of the over 3,000 needed; 115 community psychiatric nurses instead of over 3,000 required, and with only three psychiatric hospitals operating in the country” (Amoah). For these gaps to be met, the Ministry of Health must increase its budget allotted to the maintenance and more importantly the improvement of the facilities the state owns. During the fiscal year of 2007-2008 the Ministry of Health only allotted 3.95% of its budget towards mental health. That means $17,412,263 was spent that year.In a quick glance, that figure may seem like a large sum, however when broken down it means the government only spent 76 cents per capita (Raja, Shoba). The budget, within this policy, would be mandated to renovate three existing psychiatric facilities and to begin the construction of two new mental health treatment centers. It would be realistic to assert that this process would be laid out on a multiple year timeline. The most important intervention must be done within the prayer camps that are committing crimes against human rights. The renovation of the three current facilities should be timed one after the other, so only one will experience closures at any given time. Moreover, it is important that the budget continue to grow to meet the needs as Ghana transitions from three facilities to five.As it would it would be ideal for this policy to mandate to the immediate cease and closure of all prayer camps found to be in violation of human rights, however, those displaced from this closure would be refugees as they were often abandoned there in the first place. It is the recommendation of the Committee that the camps be placed on close monitoring and probation with immediate closure if crimes continue. A policy plan, that has proven successful, is to increase the amount of professionals within the country to monitor and improve these institutions. The policy did this by encouraging graduate psychology students to spend a year abroad within a developing country. By doing so, they can obtain hands on experience, complete research, and invest in the mental health capacity (Patel). This will bring in experienced conventional practitioners into the country on the University’s budget and will help reach the satisfactory amount of professionals needed to allow the individuals left at these camps to receive proper care until Ghana’s facilities can meet their citizens needs.It stands to reason that privately owned institutions and traditional practitioners who are not found to be violation of human rights may remain open but they must remain in accord with the Universal Declaration of Human Rights. Ideally, this monitoring and guidance could come from the individuals study abroad program as proposed earlier. Without the increase in capacity of Ghana’s mental health care facilities prayer camps will still arise to fill the unmet need of the citizens. options. Moreover, this policy will ensure that the funding is being used to spread the facilities throughout the inland and northern regions where prayer camps are the most common.BibliographyAe-Ngibse, Kenneth. "A Qualitative Exploration into the Widespread Use of Traditional andFaith Healers in the Provision of Mental Health Care in Ghana. “International Review of Psychiatry 22.6 (2010): 558-67. Print.Amoah, Anthony. "Four Psychiatrists for over 2 Million Mental Patients?" Ghanaian Chronicle.Web. 14 Nov. 2012.Burke, Laura. "Ghana Mental Hospital Patients Abused, Says Human Rights Watch."Huff PostWorld."Central Intelligence Agency." CIA. WORLD FACTBOOK, Web. 13 Nov. 2012.Laugharne, Richard, and Tom Burns. "The Psychiatrist." Mental Health Services in Kumasi,Ghana. 1999. 13 Nov. 2012.Medi Ssengooba "Ghana Grapples with Mental Health | Human Rights Watch." Human RightsWatch. Web. 13 Nov. 2012.“Mental Health Society of Ghana." Welcome to MHSOG. Web. 13 Nov. 2012.Patel, Virkman "Returning the Debt: How Rich Countries Can Invest in Mental Health Capacityin Developing Countries." Perspective: National Center for Biotechnology Information."Parliament Passes Mental Health Bill | Health." Parliament Passes Mental Health Bill | Health.Web. 14 Nov. 2012.Raja, Shoba. "Mapping Mental Health Finances in Ghana, Research Uganda, Sri Lanka, Indiaand Lao PDR." International Journal of Mental Health Systems 4.11 (2010)AppendicesUN General Assembly, Universal Declaration of Human Rights, 10 December 1948, 217 A (III), available at: http://www.unhcr.org/refworld/docid/3ae6b3712c.html [accessed 15 November 2012]Article 5.No one shall be subjected to torture or to cruel, inhuman or degrading treatment or punishment.Photo by tatteralan
